We know that putting a pet through surgery can be a very stressful experience. After all, we are all pet owners, and we’ve also had pets going through surgery.
Today, we pull the curtain and take you behind the scenes at LRVSS.
This is what happens to a theorical 8 year old Lab named Dakota, who needs TPLO surgery to address a torn ACL. It doesn’t really matter that he’s a dog, or what surgery he needs, since the same principles apply to almost all of our patients, cats or dog, small or large, young or old.
We chose a TPLO because it’s our most common surgery, and many other (non-TPLO) patients go through the same steps anyway.
Here is the sequence of events.
Once admitted to the hospital, Dakota gets a physical exam by the surgeon to make sure he’s healthy otherwise, and an orthopedic exam to confirm the diagnosis.
Then a picture is taken, to be featured on our Facebook page, of course assuming the owner gave us permission.

His nurse confirms that we have preop blood work and that it was reviewed by the surgeon.
If something abnormal was found, it may change our anesthesia and pain management protocol.
Dakota hops on the scale to get an accurate weight. This is important since all medications – IV or by mouth – are calculated based on his actual weight.
After a sedative and a pain medication (doggy “morphine”) are given, an IV catheter is placed. This allows giving 2 types of fluids:
- “regular” fluids (think of them as sterile saline)
- and special IV fluids that contain doggy morphine.
This allows him to receive a mini dose of morphine in every single drop.
Then Dakota walks to his run.
We do not believe in metal doors with metal bars, so each run has a glass door.

In addition, our runs are not far away “in the back,” where anything can happen.
Runs are right off the treatment room, from which nurses can see and monitor patients easily.
When it’s Dakota’s turn for surgery, he is walked outside to eliminate one last time. Then he walks to the prep area, where the nurses put him under anesthesia.
He is sandwiched between a heating pad and a fluffy blanket to maintain his temperature.
Monitoring equipment is hooked up as soon as he is sleeping.
A first dose of antibiotics is given IV.
A nurse clips the hair and prep the surgery site.
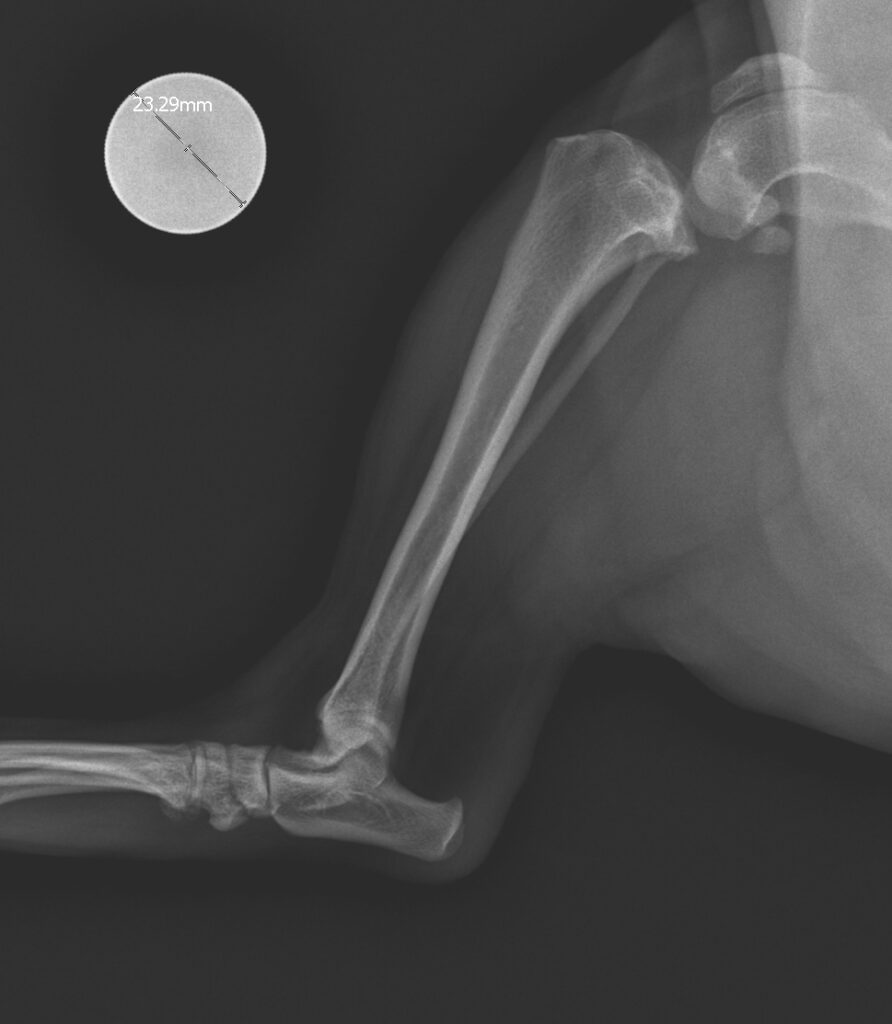
Then Dakota is placed on a gurney, which is wheeled to the X-ray table, where he is moved to another heating pad, and placed under a blanket. A different monitor is used to check his vitals while X-rays are taken.
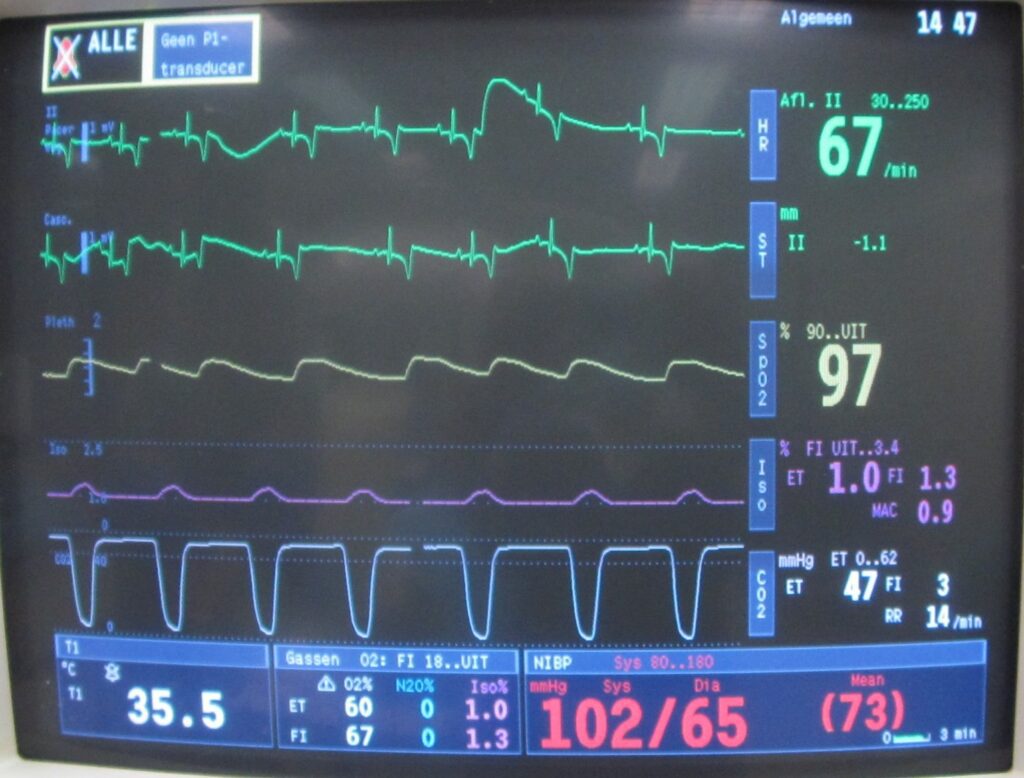
Now Dakota is wheeled into the sterile surgery room, where he is placed on a heated surgery table, covered by a nice blanket. He is covered by a human-grade heating blanket. And he is hooked up to a third monitor, which tracks half a dozen vitals throughout surgery (temperature, oxygen level, CO2 level, heart rate, respiratory rate, blood pressure).
During the entire surgery, Dakota is monitored by one of our lovely, dedicated, well-trained, anesthesia nurses. She makes a note of all vitals every 5 minutes so we can see trends, anticipate changes and keep her patient safe.
The surgery site (the knee in our case) is sterilely scrubbed by another nurse. This is a meticulous 5 minute procedure.
The surgeon then places a sterile drape over the sterile area, and surgery starts.
We will spare you the next details…
At the end of surgery, the surgeon and the nurse discuss which pain medications and antibiotics Dakota should go home on.
Once surgery is over, the surgery area is cleaned up. An antiseptic spray is applied over the incision, which is then covered with a Band-Aid.
Dakota is wheeled to the X-ray table, which is covered with a heating pad. A monitor helps to keep him safe until the very end of anesthesia. Postop X-rays are taken to make sure everything is the way it should.
He is then moved to ICU, where his anesthesia nurse continues to monitor him until he is safely awake. A plastic cone is placed around his neck before he wakes up on a yoga mat and sandwiched between fluffy blankets.

A patient wakes up after front leg surgery.
Should he need more heat support, we would add a warm-air blanket until his temperature is back up to normal.
After Dakota is awake, the anesthesia nurse calls his owners to reassure them: Dakota is recovering smoothly from anesthesia and did well in surgery.
She sets up a discharge time to send him home the next day.
IV fluids, TLC and pain medications are continued on a specific schedule on the treatment sheet.
Once Dakota is alert and standing, he can be walked outside. Later, he will be offered small amounts of water and his own food.
IV fluids, TLC and pain medications are continued throughout the night, under the close attention of his loving nurse. The fluids with the doggy morphine are slowly tapered overnight, so we can switch to oral medications.
Before Dakota can go home, IV fluids are discontinued and the IV catheter is removed.
The nurse thoroughly reviews all of the postop instructions and medications with the owner.
She shows them how to properly use the sling. She answers any additional questions. Then she helps Dakota safely get into the car if necessary.
Now the fun begins, as Dakota recovers over the next 2 months.
But we’re not done yet! We will follow his progress and help along the way, until he can enjoy life again!
As you can see, there is a lot going on behind the scenes. Everything we do is designed to keep our patients safe, loved and comfortable.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.LRVSS.com.
Never miss a blog by subscribing here: www.LRVSS.com/blog.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified
