
You’ve heard of hip dysplasia – a fancy way to say hip arthritis secondary to a deformed hip.
Well, the same can happen in an elbow.
It’s a bit more complicated, and less frequent disease.
It encompasses 3 different conditions that are occasionally found in young dogs, usually in large breeds.
Below is the story of Bruin, a beautiful and friendly 9-month-old German shepherd.
He was referred for limping in a front leg.
Why was Bruin limping?
Bruin’s owner started to train him. He seemed to be catching on very quickly. He loved to run and play. Until Bruin started to limp. He was in more and more pain over the next 4 months.
Bruin was especially friendly, and my nurses and I instantly fell in love with him.

Yet he was in serious pain.
An orthopedic exam confirmed pain in the elbow, along with a decreased range of motion.
This is very typical of elbow dysplasia, but it doesn’t tell us which of the 3 conditions is involved.
For that, we need more information through X-rays.
In a perfect world, where money is not an issue, a CAT scan would be much more precise.
Part of the reason for the increased cost is not only the much more advanced technology, but also the fact that the patient has to be under general anesthesia.
Bruin’s totally dedicated owner decided to have his puppy get pain relief through surgery.
He called “every surgeon” in upstate and downstate New York, but surgery couldn’t be done for months. “This was until I was recommended to LVRSS and Dr Zeltzman” he remembers. “Surgery could get done within a week!”
Condition #1: Un-united Anconeal Process (UAP)
This is a piece of bone that doesn’t attach properly to the ulna (aka “funny bone”), in the middle and the back of the elbow joint.
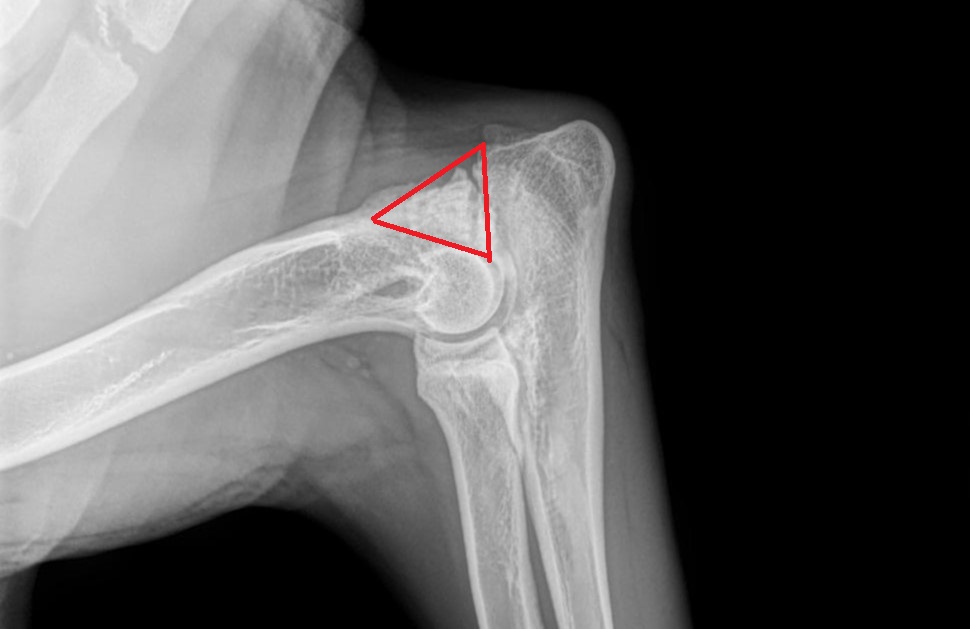
You can see it on an X-ray of the elbow before surgery.

Can you see it?
Here is the same X-ray, with a red arrow showing the separation in the bone.

Can you see it now?
Here is the same X-ray, with a red triangle around the UAP.
After a short incision was made on the outside of the elbow, the UAP was removed.
It was a huge piece of bone as you can see below, almost the size of a quarter. Although there is a technique where the UAP can be reattached to the main part of the bone, it was deemed preferable to remove it in Bruin’s case.

Here is the X-ray of the elbow after surgery, after the big piece of UAP bone was removed (see red arrow that shows that a big triangle of bone is now missing).

After seeing the UAP fragment, Bruin’s owner commented: “I was in shock when I saw the size of the bone. I couldn’t believe he was walking around with that thing in his elbow!”
But wait, there’s more!
Condition #2: Fragmented Coronoid Process (FCP)
An FCP is also a piece of bone that doesn’t attach properly to the ulna (funny bone), on the inside of the elbow.
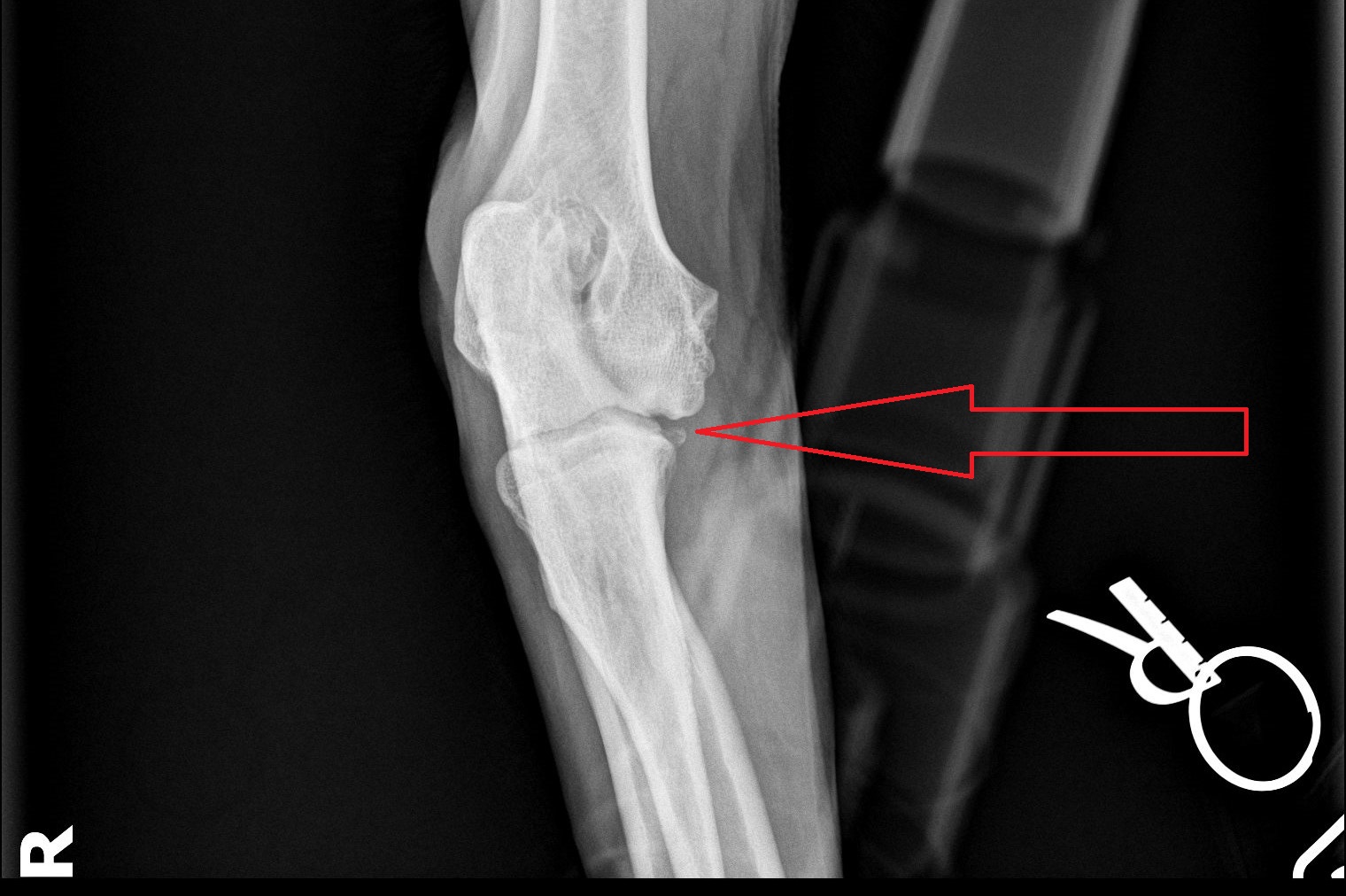
This is sometimes tricky to see on X-rays. In fact, we almost never see it. We more often see hints that there is an issue in that area.
In Bruin’s case, we could see a hint of a tiny fragment (see red arrow).
A small incision was made on the inside of the elbow.
We actually found not 1, but 2 big fragments as you can see in the picture below, next to a scalpel blade.
The blade is 37 mm, or 1.5 inches long, for comparison.
Now you can see how misleading an X-ray can be: it showed 1 possible tiny FCP, when in fact we removed 2 large fragments.
When he saw the 2 FCP fragments, Bruin’s owner said: “Knowing that stuff is out of his elbow is such a relief. I’m positive he is feeling better on this leg!”
But wait, there’s more!

Condition #3: Osteo-Chondritis Dissecans (OCD)
It is always important to explore the elbow joint to make sure there is nothing else going on.
And sure enough, we found and removed a piece of cartilage inside the elbow.
So poor Bruin had all 3 parts of elbow dysplasia!
I always compare a UAP, an FCP or an OCD lesion to having a pebble in your shoe.
I can’t even imagine how Bruin must have felt with all 3 (actually 4) “pebbles” moving around at every step!
Yet he remained incredibly sweet, loving, and playful.
We finished surgery and Bruin recovered smoothly from anesthesia.
His owner remembers: “After surgery, Dr. Zeltzman called me and I was relieved to hear that surgery was a success.”
Our shepherd pup went home the next day with pain medications, antibiotics, and high-quality arthritis supplements.
“I didn’t think he would be able to walk for a while. Yet, the next morning, as the overnight nurse walked Bruin out, I was excited and happy to see him walking!” commented his owner.
He now needed very strict rest, physical therapy of the elbow, and short leash walks for 8 weeks.
But Bruin did so well, that we stopped his confinement after only 1 month.
We slowly increased his activity level, indoors and outside, over the following month.
And after that, he was able to resume his normal, crazy, happy puppy life.
His owner commented: “He is clearly much happier. He has not cried in pain since surgery. He is full of energy!
For the first time since finding out about the condition, I am confident Bruin will be able to live a good, happy, healthy life with proper management of the condition.
I am very thankful for how quickly I was able to get him into surgery.”
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.LRVSS.com
Never miss a blog by subscribing here: www.LRVSS.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified
